The Sioux Lookout Protocol
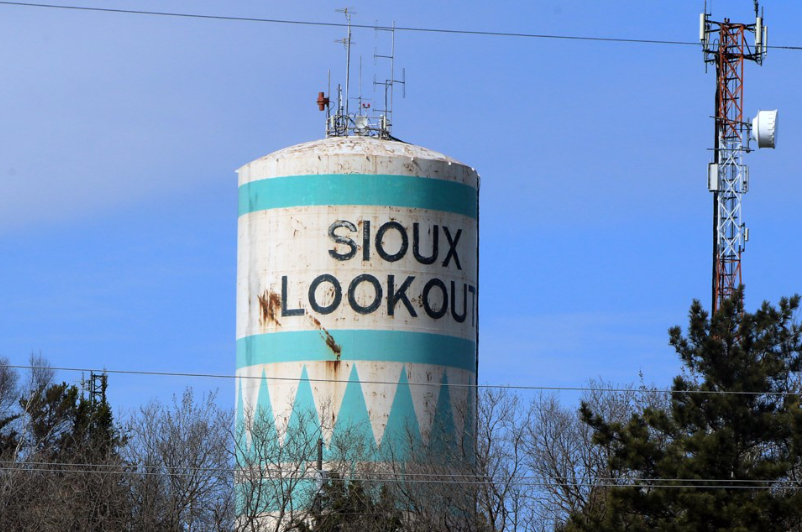
Case Study: Engineering a 1,300% Capacity Increase in a Zero-Sum Market
Executive Snapshot
The Problem
34 remote, fly-in Indigenous communities facing chronic physician vacancies.
The Constraints
A zero-sum talent market.
High clinician burnout.
Extreme geography and operational fragility.
The Result
Scaled the active provider network by 1,300% over four years—without increasing market supply.
The Diagnosis
Traditional recruitment logic breaks down in remote healthcare.
The default response is to increase funnel volume: more ads, more outreach, more urgency.
In this environment, volume is irrelevant.
When churn exceeds intake, recruitment becomes a leaky bucket.
You don’t have a sourcing problem—you have a system stability problem.
So the first shift was diagnostic, not tactical.
I stopped optimizing for Time-to-Fill
and started optimizing for Psychological Safety Duration.
The core question changed from:
“How fast can we place someone?”
to:
“How long can we keep them safe, supported, and effective once they arrive?”
The Protocol
We redesigned the system around retention through stability, not attraction through pressure.
1. De-Risking Entry
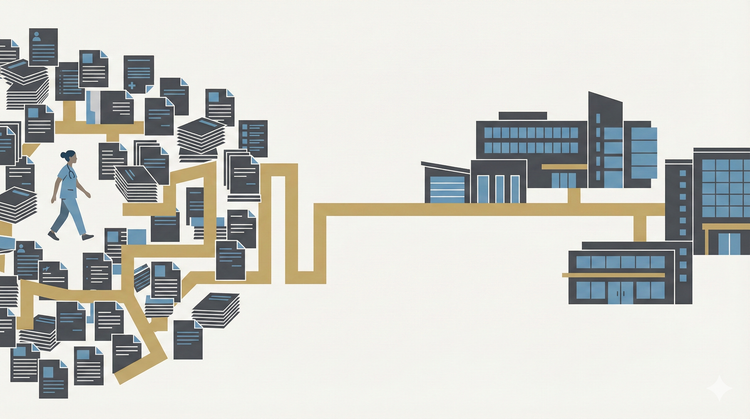
We built a standardized onboarding ramp that removed the majority of non-clinical friction.
Licensing, logistics, scheduling, and community orientation were handled upstream—before arrival.
The goal wasn’t speed.
It was predictability.
When clinicians knew what to expect, anxiety dropped and early exits declined.
2. The Psychological Safety Loop
Placement alone wasn’t enough.
We implemented a rapid-response operational support layer so clinicians were insulated from bureaucratic failure in real time.
Problems were addressed before they became resignation triggers.
Physicians weren’t just placed into communities.
They were held by the system.
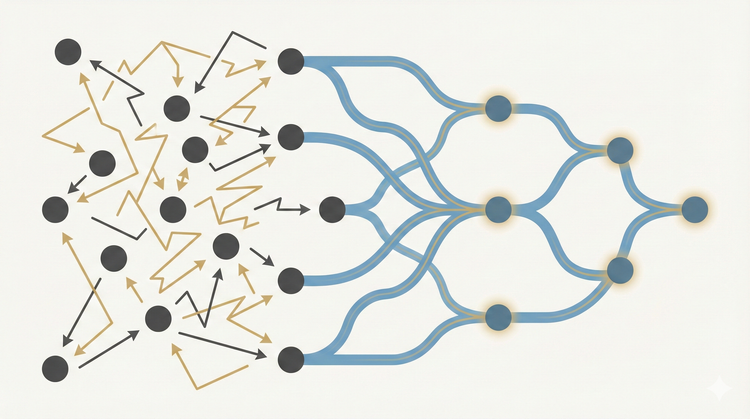
3. Network Effects at Scale
We centralized the locum model into a regional pool (NOHRA), allowing clinicians to rotate between communities.
This created three compounding effects:
- Burnout decreased through planned circulation
- Coverage stabilized across the region
- Trust increased as clinicians stayed within a familiar system
The system became adaptive instead of brittle.
The Outcome
- 1,300% increase in deployed clinical FTE capacity
- Significant reduction in agency dependency
- Sustained regional coverage without increasing market supply
Media coverage: CBC feature on system transformation
The Asymmetric Insight
This wasn’t a recruitment win.
It was a system design correction.
In constrained markets, hiring is not about persuasion.
It’s about removing fear, friction, and fragility from the operating environment.
This protocol—stabilize first, scale second—is the foundation of the asymmetric leverage model I use today when healthcare systems are under acute stress.
Fix the system, and capacity follows.
Chase volume, and the system collapses faster.